
Mania vs hypomania is a comparison often discussed in relation to mood disorders, particularly bipolar disorder. While they share similarities, understanding the nuances between mania and hypomania is crucial for accurate diagnosis and appropriate treatment.
Mania and hypomania both involve periods of elevated mood, energy, and activity levels, but they differ in intensity, duration, and impact on daily functioning. These states can profoundly affect individuals’ lives, influencing their relationships, work, and overall well-being.
For those experiencing these episodes, navigating the highs and lows can be challenging, highlighting the importance of awareness and support in managing these conditions effectively.
Understanding Mania
Understanding mania is essential in grasping its implications on mental health. Mania is a defining characteristic of bipolar disorder, characterized by a distinct period of abnormally and persistently elevated, expansive, or irritable mood, along with increased energy and activity levels. During manic episodes, individuals may experience racing thoughts, reduced need for sleep, grandiose beliefs about their abilities, and engaging in risky behaviors such as excessive spending or reckless driving.
These symptoms often interfere with daily functioning and can lead to significant impairment in various aspects of life, including relationships, work, and personal safety.
Mania Symptoms
Mania symptoms encompass a wide range of experiences that significantly impact an individual’s behavior, emotions, and cognition. These symptoms often manifest in distinct ways, indicating a departure from typical functioning. Some common signs of mania include:
- Persistent elevated or euphoric mood
- Increased energy and activity levels
- Reduced need for sleep without feeling tired
- Racing thoughts or rapid speech
- Grandiosity or inflated sense of self-esteem
- Impulsivity and engaging in risky behaviors such as excessive spending, substance abuse, or reckless driving
- Difficulty concentrating or focusing on tasks
- Irritability or agitation when others attempt to intervene or restrict their activities
These symptoms can vary in intensity and duration but collectively contribute to the disruptive nature of manic episodes. It’s essential to recognize these signs and seek professional evaluation and support for appropriate management.
Causes of Mania
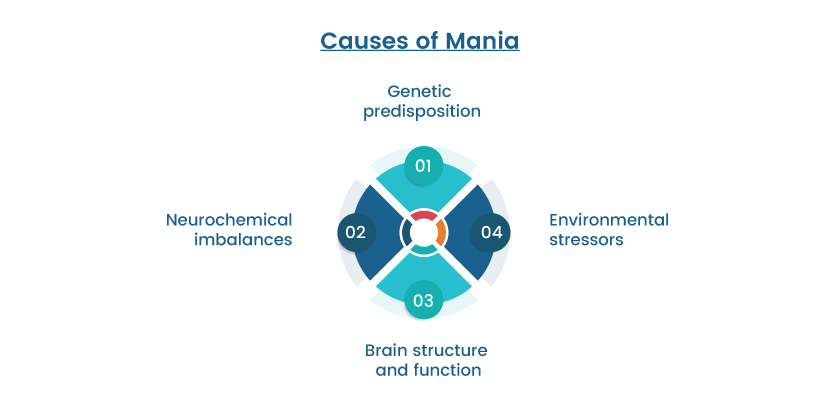
The causes of mania are complex and multifaceted, often involving a combination of genetic, biological, and environmental factors. While the exact mechanisms underlying mania remain the subject of ongoing research, several key contributors have been identified:
Genetic predisposition: There is evidence to suggest that bipolar disorder, including manic episodes, has a hereditary component. Individuals with a family history of bipolar disorder are at an increased risk of developing the condition themselves.
Neurochemical imbalances: Imbalances in neurotransmitters such as dopamine, serotonin, and norepinephrine are thought to play a role in the development of mania. Disruptions in these brain chemicals can affect mood regulation and lead to episodes of mania.
Brain structure and function: Differences in the structure and function of certain brain regions, including the prefrontal cortex and limbic system, have been observed in individuals with bipolar disorder. These abnormalities may contribute to the onset and expression of manic symptoms.
Environmental stressors: Stressful life events, such as trauma, loss, or significant life changes, can trigger manic episodes in susceptible individuals. Additionally, disruptions in sleep patterns, substance abuse, and other environmental factors can exacerbate symptoms of mania.
What are the 3 Types of Mania
Mania is typically categorized into three distinct types, each characterized by its duration, severity, and associated features:
Bipolar I Disorder:
This type of mania involves full-blown manic episodes lasting for at least seven days or requiring hospitalization due to their severity. Individuals with bipolar I disorder may also experience depressive episodes, which alternate with manic episodes or occur independently.
Bipolar II Disorder:
In bipolar II disorder, individuals experience hypomanic episodes, which are less severe than full manic episodes but still involve elevated mood, increased energy, and other manic symptoms. Hypomanic episodes typically last for at least four days and are often followed by depressive episodes.
Cyclothymic Disorder
Cyclothymic disorder is characterized by recurrent periods of hypomanic symptoms and depressive symptoms that do not meet the criteria for a full manic or depressive episode. These mood fluctuations are less severe than those seen in bipolar I and II disorders but can still significantly impact daily functioning over an extended period.

Understanding Hypomania
Understanding hypomania is crucial in recognizing its significance within the spectrum of mood disorders. So what is hypomania? Hypomania shares similarities with mania but is distinguished by its milder intensity and shorter duration. Individuals experiencing hypomanic episodes typically exhibit elevated mood, increased energy, and heightened creativity or productivity.
Unlike full-blown manic episodes, hypomania does not typically cause severe impairment in social or occupational functioning, although it can still lead to impulsive or risky behaviors.
It’s important to note that while hypomania may feel euphoric or energizing to those experiencing it, it can also be a sign of underlying mental health conditions such as bipolar II disorder.
Symptoms of Hypomania
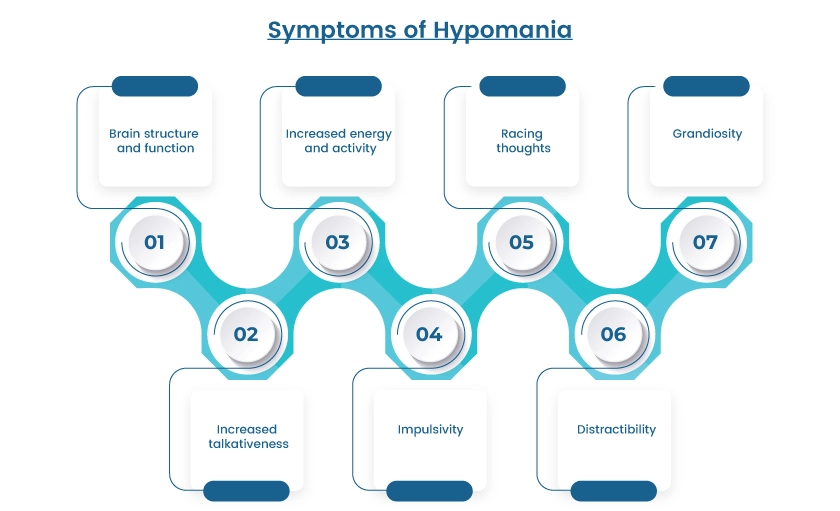
Symptoms of hypomania encompass a range of experiences that reflect elevated mood and increased activity levels, although to a lesser degree than full-blown mania. Individuals experiencing hypomanic episodes may exhibit the following signs:
Elevated or expansive mood: A pervasive sense of euphoria, happiness, or irritability that is uncharacteristic of the person’s typical mood.
Increased energy and activity: A noticeable surge in energy levels, leading to heightened productivity, restlessness, and a decreased need for sleep.
Racing thoughts: Rapid, disjointed thoughts that may be difficult to control or focus on, contributing to a sense of mental agitation.
Grandiosity: Exaggerated beliefs about one’s abilities, talents, or importance, leading to inflated self-esteem or confidence.
Increased talkativeness: A tendency to speak rapidly and excessively, often jumping from one topic to another without pause.
Impulsivity: Acting on impulses or engaging in risky behaviors such as excessive spending, substance abuse, or reckless driving without considering the consequences.
Distractibility: Difficulty concentrating or staying focused on tasks due to an abundance of thoughts or external stimuli.
Mania VS Hypomania
Mania and hypomania are both characterized by periods of elevated mood and increased energy levels, but they differ in terms of severity, duration, and impact on daily functioning. While mania represents a more intense manifestation of these symptoms and often leads to significant impairment in various aspects of life, hypomania is generally milder and may not cause as much disruption.
Understanding the distinctions between mania and hypomania is essential for accurate diagnosis and appropriate treatment. Below is a comparison table highlighting the key differences between the two states:
| Feature | Mania | Hypomania |
| Duration | Typically lasts for at least seven days or may require hospitalization | Generally lasts for at least four days |
| Severity | Severe symptoms causing significant impairment | Symptoms are milder and may not impair functioning as severely |
| Impulsivity | Often accompanied by impulsive or risky behaviors | May involve some impulsivity but typically less severe |
| Psychosis | Can involve psychotic features such as delusions or hallucinations | Usually does not involve psychotic features |
| Impact on life | Often disrupts relationships, work, and daily activities | May lead to some disruption but generally less severe |
| Diagnosis | Characteristic of Bipolar I Disorder | Characteristic of Bipolar II Disorder |
Management and Treatment
Managing and treating mania and hypomania typically involves a combination of medication, psychotherapy, lifestyle changes, and support from healthcare professionals. Here are eight treatment options commonly utilized:
Medication: Mood stabilizers such as lithium, antipsychotics, and anticonvulsants are often prescribed to help stabilize mood and reduce the frequency and severity of manic or hypomanic episodes. In some cases, advanced options like TMS therapy or telepsychiatry may also support long-term management.
Psychotherapy: Cognitive-behavioral therapy (CBT) and psychoeducation can help individuals better understand and manage their symptoms, develop coping strategies, and identify triggers for mood episodes.
Mood Tracking: Keeping a mood journal or using mood-tracking apps can help individuals monitor their symptoms, identify patterns, and communicate effectively with healthcare providers.
Sleep Management: Maintaining a regular sleep schedule and practicing good sleep hygiene can help stabilize mood and reduce the risk of manic or hypomanic episodes triggered by sleep disturbances.
Stress Reduction Techniques: Learning stress management techniques such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help reduce the impact of stressors on mood.
Limiting Stimulants: Avoiding or limiting the consumption of stimulants such as caffeine and nicotine can help reduce the risk of exacerbating manic or hypomanic symptoms.
Regular Exercise: Engaging in regular physical activity has been shown to have mood-stabilizing effects and can help reduce symptoms of mania and hypomania.
Social Support: Building a strong support network of family, friends, and mental health professionals can provide emotional support, encouragement, and assistance in managing symptoms and adhering to treatment plans.
These treatment options may be used alone or in combination, depending on the individual’s specific needs and preferences. It’s essential for individuals experiencing manic or hypomanic symptoms to work closely with their healthcare team to develop a comprehensive treatment plan tailored to their unique situation.
Manic vs Hypomanic
Individuals experiencing mania may exhibit psychotic features such as delusions or hallucinations, whereas hypomania generally does not involve psychotic symptoms.
The duration of manic episodes is typically longer, lasting at least seven days, whereas hypomanic episodes are shorter, lasting at least four days. In clinical discussions, this difference is often framed as hypomanic vs manic.
| Feature | Manic Episode | Hypomanic Episode |
| Severity | Severe symptoms, often requiring hospitalization | Milder symptoms, less likely to require hospitalization |
| Duration | Typically lasts for at least seven days | Typically lasts for at least four days |
| Psychotic Features | May involve psychotic symptoms such as delusions or hallucinations | Typically does not involve psychotic symptoms |
Hypomanic vs Hypermanic
Hypermania represents an extreme form of mania, often accompanied by severe psychotic features and significant impairment in functioning. While hypomania may lead to some disruption in daily life, hypermania typically results in profound impairment and may require urgent intervention.
| Feature | Hypomanic Episode | Hypermanic Episode |
| Severity | Milder symptoms compared to hypermania | Extreme symptoms, often requiring urgent intervention |
| Psychotic Features | Typically does not involve psychotic features | May involve severe psychotic symptoms such as delusions or hallucinations |
| Impact on Life | May lead to some disruption in daily life | Results in profound impairment and significant disruption |
Mania vs Hypomania DSM
Mania is characterized by a distinct period of abnormally and persistently elevated, expansive, or irritable mood, lasting at least one week, according to the DSM-5 criteria.
Both mania and hypomania are key features in diagnosing bipolar I and II disorders, respectively, as outlined in the DSM-5.
| DSM Criteria | Mania | Hypomania |
| Duration | At least one week | At least four days |
| Severity | Severe symptoms causing significant impairment | Milder symptoms, may not cause significant impairment |
| Diagnosis | Characteristic of Bipolar I Disorder | Characteristic of Bipolar II Disorder |
Ending Note
Understanding the difference between mania and hypomania is crucial for accurately diagnosing and effectively managing mood disorders such as bipolar disorder. While both states involve periods of elevated mood and increased energy levels, they vary in severity, duration, and impact on daily functioning. Manic episodes are more severe and may require hospitalization, while hypomanic episodes are milder and typically do not cause significant impairment.
By recognizing the signs and symptoms of mania and hypomania and utilizing appropriate treatment options, individuals can better navigate the challenges posed by these mood disturbances and work towards achieving greater stability and well-being in their lives.




